Background: Peripheral T cell lymphoma (PTCL) and Extranodal NK/T cell lymphoma (ENKTCL) are rare types of non-Hodgkin's lymphoma (NHL), with a higher incidence in Asian countries. Outcomes for patients with relapsed or refractory (R/R) PTCL and ENKTCL are very poor. There is still a lack of effective treatment for these patients. Mitoxantrone is a synthetic anthracenedione anti-cancer drug that is effective in lymphoma, leukemia, and other solid tumors. Liposome preparations have shown higher anti-tumor effect and lower toxicities due to modified drug release and particle shape. Mitoxantrone hydrochloride liposome (PLM60) was manufactured by Shijiazhuang Pharmaceutical Group Co., Ltd. (CSPC). High accumulation in tumor tissue was a key characteristic of PLM60 in our preclinical investigation. The pharmacokinetic parameters, especially half-life of PLM60 was prolonged significantly in phase Ⅰ trial. Phase II exploratory clinical trial showed promising results in R/R PTCL. Therefore, we conducted this pivotal registration phase II trial to evaluate the efficacy and safety of PLM60 in patients with R/R PTCL and ENKTCL. At the present time, this was the first clinical trial to assess PLM60 in treating R/R PTCL and ENKTCL worldwide.
Methods: This was a prospective, single-arm, open-label, multi-center, phase II clinical trial. Adult patients with histologically confirmed PTCL (mainly peripheral T cell lymphoma, NOS, PTCL-NOS; angioimmunoblastic T-cell lymphoma, AITL; anaplastic large cell lymphoma, ALCL) after prior anthracyclines-based chemotherapy or ENKTCL failed from asparaginase-contained regimen, ECOG performance status ≤ 1, adequate organ function and bone marrow function, and at least one measurable or evaluable lesion were recruited in this trial. Main exclusion criteria were patients with a cumulative dose of doxorubicin >360 mg/m2, known history of a clinically significant cardiac malfunction or uncontrollable cardiovascular diseases. PLM60 20mg/m2 was administered intravenously every 4 weeks. Treatment may continue for up to 6 cycles or until disease progression, or intolerable toxicity. The primary endpoint was objective response rate (ORR) based on Independent Review Committee (IRC) assessments according to Revised Response Criteria for Malignant Lymphoma (version 2007). Secondary endpoints included ORR based on assessment between investigators, duration of response (DoR), progression-free survival (PFS), overall survival (OS), disease control rate (DCR), and safety. Adverse events were rated according to the NCI Common Terminology Criteria for Adverse Events (CTCAE) 4.03. This trial is registered at ClinicalTrials.gov (NCT03776279).
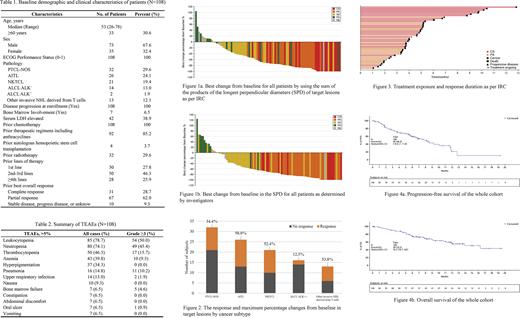
Results: One hundred and eight eligible patients were treated in 26 institutions in China between April 26, 2018 and May 19, 2020. Patient characteristics are summarized in Table 1. 98 patients were evaluable for response. 44 patients (40.7%, 95% CI, 31.4-50.6%) achieved an objective response including 22 (20.4%) patients achieved CR based on IRC assessment (Figure 1a). ORR were 34.4% (11/32), 50.0% (13/26), 52.4% (11/21), 12.5% (2/16) , 53.8% (7/13) and the CR rates were 18.8% (6/32), 23.1% (6/26), 28.6% (6/21), 6.3% (1/16), 23.1% (3/13) for PTCL-NOS, AITL, NKTCL, ALCL ALK+/-, and other subtypes , respectively (Figure 2). The ORR for patients who received at least 2 cycles of treatment (N=90) was 60.0% (95% CI, 49.1-70.2%). The investigator-evaluated ORR for the whole cohort was 43.5% (95% CI, 34.0-53.4%) (Figure 1b). Median DCR of all patients was 77.8% (95% CI, 68.8-85.2%). The median DoR of the whole group was 9.8 (95% CI, 5.1-not evaluated) months. 77.3% (34/44) of patients achieved response had a DoR ≥3 months (Figure 3). Median PFS of the whole cohort was 6.7 (95% CI, 5.5-10.4) months, with a 6-month PFS rate of 55.3% (95% CI, 44.5-64.8%). Median OS of the whole group was 16.3 (95% CI, 10.7-not evaluated) months, with a 6-month OS rate of 74.9% (95% CI, 64.9-82.4%) (Figure 4a, 4b). All-grade treatment-emergent adverse events (TEAEs, >5%) are listed in Table 2. The most common toxicities of PLM60 were hematological toxicities. The most common grade ≥3 toxicities were leukocytopenia (50.0%) and neutropenia (45.4%).
Conclusion: PLM60 monotherapy yielded promising results for patients with R/R PTCL and ENKTCL with moderate toxicities. Further investigation of combination therapy is warranted.
Xia:CSPC ZhongQi Pharmaceutical Technology (Shijiazhuang) Co., Ltd.: Current Employment. Xue:CSPC ZhongQi Pharmaceutical Technology (Shijiazhuang) Co., Ltd.: Current Employment. Li:CSPC ZhongQi Pharmaceutical Technology (Shijiazhuang) Co., Ltd.: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal